MASSAGE
Getting The Most Out of Your Massage
You can help get the most out of your session by arriving on time so we can ensure each client gets the attention they deserve. Before your massage service, it is best to let your therapist know what you like and what you want. Let your therapist know if the room is too cold or warm for your comfort, or if you would like the music louder or softer.
Some clients like to chat during their session and others prefer it to be quiet, it is perfectly ok to do either. Don’t be shy, feel free to insist on getting exactly what you need, including silence. You won’t hurt anyone’s feelings if you share your preferences in a clear and pleasant way. Your satisfaction is our number one priority!
Regular Massage Treatments

Swedish Massage
Light to firm pressure which increases oxygen flow in the blood releasing toxins from muscles & eases tension from daily stress.
- Increases level of oxygen in blood and lowers muscle toxins
- Increase circulation and flexibility

Deep Tissue Massage
Manipulation of superficial and deeper layers of muscle and connective tissue to relieve pain and restore normal movement.
- Reduces blood pressure and stress hormone levels
- Releases chronic muscle tension

Sports Massage
A deep tissue massage combined with stretching of muscles and joints.
- Promotes flexibility and reduces fatigue
- Improves endurance

Neuromuscular / Trigger Point Massage
Pressure is applied to soft tissue to concentrate on and relieve chronic muscular pain by using pressure to trigger points of referred pain.
- Significantly decreases pain after one treatment
- Releases constricted areas

Pre-Natal Massage
Reduces stress and tension and enhances pliability of the skin and tissue. (After 1st Trimester Only)
- Reduces stress on weight-bearing joints and promotes lymph and blood circulation
- Relaxes nervous tension
Speciality Massages

Reflexology
Pressure applied to reflex areas on feet corresponding to glands, organs, and body parts. Reflexology can cleanse the body of toxins, and increase circulation.
- Helps relieves pain in upper leg, calf, and foot
- Helps decrease stress and anxiety

Hot Stone Treatment
A relaxing treatment involving a series of gentle strokes using warm basalt stones and oil. Adding heat to specific areas on the body enhances the feelings of relaxation and peace. The stones can be used to massage areas of the body.
- Deeper muscle relaxation and encourages blood flow throughout body

Connective Tissue Massage
Releases myofascial restrictions, relieves chronic tension, produces greater efficiency of movement, improves posture, and increases body awareness.
- Releases connective tissue restrictions in body and breaks up restrictive scar tissue
- Relieves chronic tension
Advanced Clinical Massages

Medical Massage
The application of specific treatment protocols targeted to the specific problem(s), and focuses on using purely therapeutic medical massage techniques.
- Increases recovery time for particular problem
- Targeted to specific problem areas

Structural Integration
A 10 session series developed by Dr. Ida P. Rolf. The system produces lasting relief of chronic tension, creates greater fluidity of movement, and allows for an effortless upright posture. The therapist will massage areas outward and in toward the heart and vital organs.
- Increases range of motion and decreases pain
Massage Enhancements

Aromatherapy
Aromatherapy uses oils from herbs, flowers, and fruits to relax the mind & body.
- Enhances the benefits of massage
- Helps with anxiety release

Bio Freeze
A cooling gel used to provide pain relief for sore muscles and stiff joints.
- Leaves muscles feeling stimulated and invigorated
- Helps to release tension and decrease pain
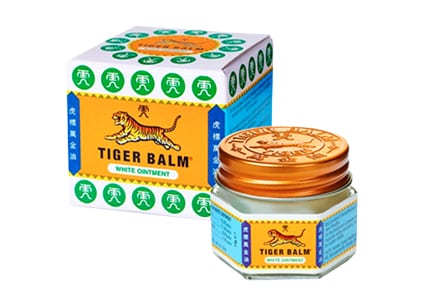
Tiger Balm
A warm soothing relief ointment rub for everyday aches and pains.
- Used as massage oil for muscle soreness from exercise
- Helps relieve muscle and joint pain
Massage Techniques & Modalities
Massage
People of all ages, lifestyles, and professions come to Holistic Massage and Wellness Clinics seeking relaxation, stress reduction, or injury relief. We consider massage an essential factor in any health care routine. Find the perfect massage therapy in Hollywood FL that fits your Holistic health care needs!
Benefits of Massage
Our rejuvenating massages are an integral part of your healthy lifestyle. The ancient art of massage has been used throughout the centuries to soothe aches and pains and facilitate the body’s own healing powers. With today’s busy, stressful lifestyles, there’s never been a better time to take advantage of the benefits of massage therapy.
Benefits of Massage include:
- Relieves stress
- Lowers blood pressure
- Increases blood circulation and lymph flow
- Relaxes muscles
- Improves range of motion
- Increases endorphins (the body’s natural painkillers)
- May enhance medical treatment
- Helps people feel less anxious and stressed, relaxed yet more alert
- Creates a sense of well-being
- Relieves muscle tension and stiffness
- Strengthens the immune system
- Improves flexibility
- Relieves pain
Routine massage can have the ability to addresses the following ailments:
- Arthritis
- Cancer
- Depression and Anxiety
- Fibromyalgia and Chronic Fatigue Syndrome
- Heart Disease and Other Stress-Related Pathologies
- Other Conditions
Therapeutic Aromatherapy
Aromatherapy is the use of plant oils to alleviate physical and psychological disorders. They work in two ways: through massage and skin absorption, and through inhalation and the respiratory system. The therapeutic effects of aromatherapy oils vary; some oils have an sedative effect while others are more stimulating. Aromatherapy can help you achieve the state of mind and body you desire. Aromatherapy relaxes tight and tense muscles and facilitates stimulation of blood and lymph circulation.
